By Carol Stoll
Hearing loss is one of the most prevalent chronic conditions in the U.S. and has been associated with negative physical, social, cognitive, economic, and emotional consequences. Despite the high prevalence of hearing loss, substantial gaps in the utilization of amplification options, including hearing aids and cochlear implants (CI), have been identified. Harrison Lin, M.D., a 2016 Emerging Research Grants recipient, along with colleagues, recently published a paper in JAMA Otolaryngology–Head & Neck Surgery that investigates the contemporary prevalence, characteristics, and patterns of specialty referral, evaluation, and treatment of hearing difficulty among adults in the U.S.
Unlike this man who is having his hearing tested, a large number of individuals in the U.S. who experience hearing difficulties are not seeking treatment. Photo source: Bundesinnung Hörakustiker, Flickr.
The researchers did a cross-sectional analysis of responses from a nationwide representative sample of adults who participated in the 2014 National Health Interview Survey and responded to hearing health questions. The data collected included demographic information as well as self-reported hearing status, functional hearing, laterality (hearing ability in each ear), onset, and primary cause (if known) of the hearing loss. In addition, the team analyzed specific data regarding hearing-related clinician visits, hearing tests, referrals to hearing specialist, and utilization of hearing aids and CIs.
Overall, 36,690 records were included in the analysis, which extrapolated to an estimated 239.6 million adults in the U.S. Nearly 17 percent indicated their hearing was less than “excellent/good,” ranging from “a little trouble hearing” to “deaf.” Approximately 21 percent of respondents had visited a physician for hearing problems in the preceding five years. Of these, 33 percent were referred to an otolaryngologist and 27 percent were referred to an audiologist. Of the adults who indicated their hearing from “a little trouble hearing” to being “deaf,” 32 percent had never seen a clinician for hearing problems and 28 percent had never had their hearing tested.
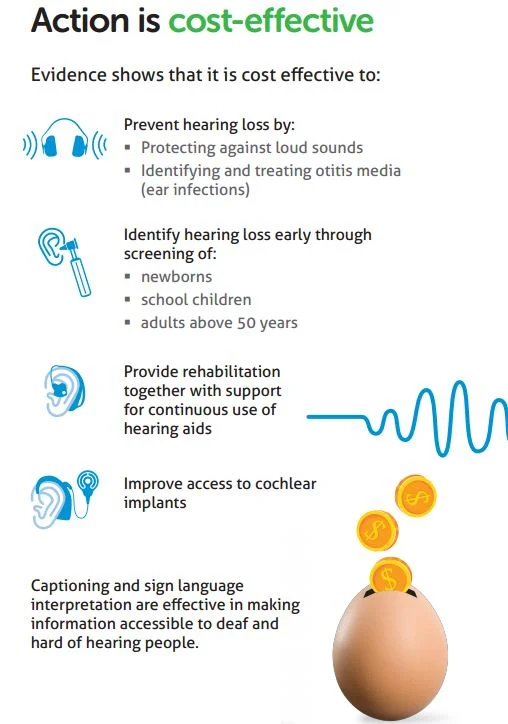
The study shows that there are considerable gaps between self-reported hearing loss and patients receiving medical evaluation and recommended treatments for hearing loss. Increased awareness among clinicians regarding the burden of hearing loss, the importance of early detection and medically evaluating hearing loss, and available amplification and CI options can contribute to improved care for individuals with hearing difficulty. Future studies are warranted to further investigate the observed trends of this study.
Harrison W. Lin, M.D., is a 2016 Emerging Research Grants recipient. His grant was generously funded by funded by The Barbara Epstein Foundation, Inc.
We need your help supporting innovative hearing and balance science through our Emerging Research Grants program. Please make a contribution today.