One way to help all those with hearing conditions is to become a Research Pioneer, a special group of friends who give a monthly gift to support HHF. Research Pioneers provide predictable funding we can count on to fund life-changing scientific breakthroughs.
Mapping Better Hearing
By Vicky Chan
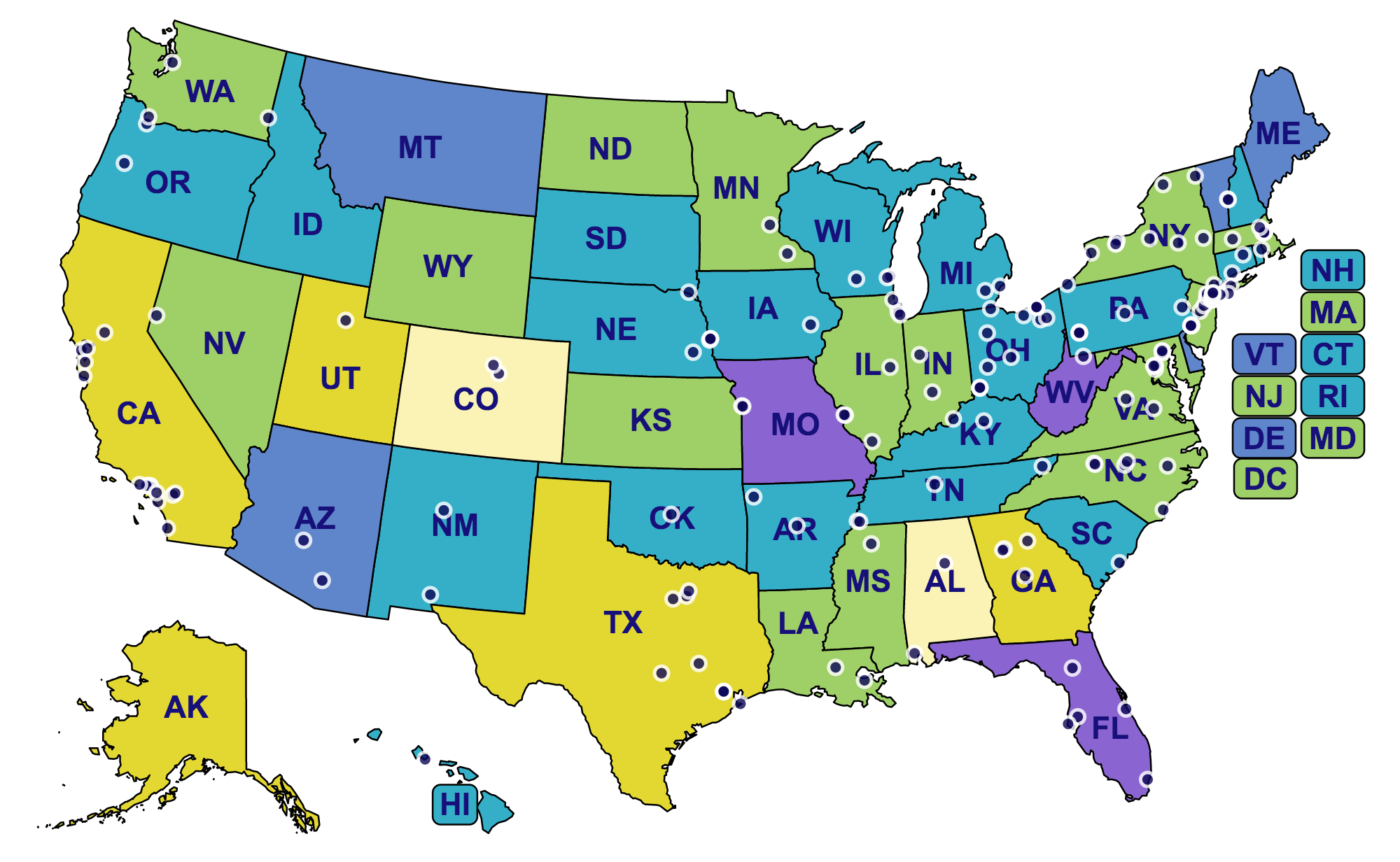
Hearing Health Foundation (HHF) is grateful to the many individuals and organizations who have empowered groundbreaking hearing loss research in the last 60 years. A new interactive map displays every institution in the U.S. where HHF has been fortunate to fund groundbreaking research, yielding outstanding advancements in hearing and balance science. The map also indicates the rates of hearing loss in each state, signaling that additional work is urgently needed.
The colors—light yellow, yellow, green, teal, blue, and purple—represent the rates of hearing loss in each state. The calculations are based off 2015 U.S. Census Data, using estimates from the well-known prevalence of hearing loss among specific demographics. At the lowest end of the range in light yellow, hearing loss affects 13.71% of Colorado’s population. The highest rate was found in Missouri, purple, where the prevalence measured 20.15%. The mean for all states was 18.16%. The numbers signal the significance of hearing loss research.
Nearly all of the institutions on the map represent recipients of the Emerging Research Grants (ERG) who have carried out investigations related to tinnitus, hyperacusis, Ménière's disease, Usher syndrome, hearing loss in children, Central Auditory Processing Disorder, and strial atrophy.
A few institutions are home to the work of the Hearing Restoration Project’s (HRP) domestic consortium members, who focus on investigating hair cell regeneration as a cure for hearing loss and tinnitus. They conduct research at Baylor College of Medicine, Harvard Medical School, Oregon Health & Science University, Stanford University, Stowers Institute, University of Maryland, University of Michigan, University of Southern California, University of Washington, and Washington University.
By mid-year, the institutions corresponding to HHF’s newly formed Ménière's Disease Grants (MDG) program will be added to the map.
HHF envisions a world in which no one lives with hearing loss and tinnitus—until this is realized, we’ll do everything we can to put more innovative hearing loss research on the map.
The Gap Between Self-Reported Hearing Loss and Treatment Patterns
By Carol Stoll
Hearing loss is one of the most prevalent chronic conditions in the U.S. and has been associated with negative physical, social, cognitive, economic, and emotional consequences. Despite the high prevalence of hearing loss, substantial gaps in the utilization of amplification options, including hearing aids and cochlear implants (CI), have been identified. Harrison Lin, M.D., a 2016 Emerging Research Grants recipient, along with colleagues, recently published a paper in JAMA Otolaryngology–Head & Neck Surgery that investigates the contemporary prevalence, characteristics, and patterns of specialty referral, evaluation, and treatment of hearing difficulty among adults in the U.S.
Unlike this man who is having his hearing tested, a large number of individuals in the U.S. who experience hearing difficulties are not seeking treatment. Photo source: Bundesinnung Hörakustiker, Flickr.
The researchers did a cross-sectional analysis of responses from a nationwide representative sample of adults who participated in the 2014 National Health Interview Survey and responded to hearing health questions. The data collected included demographic information as well as self-reported hearing status, functional hearing, laterality (hearing ability in each ear), onset, and primary cause (if known) of the hearing loss. In addition, the team analyzed specific data regarding hearing-related clinician visits, hearing tests, referrals to hearing specialist, and utilization of hearing aids and CIs.
Overall, 36,690 records were included in the analysis, which extrapolated to an estimated 239.6 million adults in the U.S. Nearly 17 percent indicated their hearing was less than “excellent/good,” ranging from “a little trouble hearing” to “deaf.” Approximately 21 percent of respondents had visited a physician for hearing problems in the preceding five years. Of these, 33 percent were referred to an otolaryngologist and 27 percent were referred to an audiologist. Of the adults who indicated their hearing from “a little trouble hearing” to being “deaf,” 32 percent had never seen a clinician for hearing problems and 28 percent had never had their hearing tested.
The study shows that there are considerable gaps between self-reported hearing loss and patients receiving medical evaluation and recommended treatments for hearing loss. Increased awareness among clinicians regarding the burden of hearing loss, the importance of early detection and medically evaluating hearing loss, and available amplification and CI options can contribute to improved care for individuals with hearing difficulty. Future studies are warranted to further investigate the observed trends of this study.
Harrison W. Lin, M.D., is a 2016 Emerging Research Grants recipient. His grant was generously funded by funded by The Barbara Epstein Foundation, Inc.
We need your help supporting innovative hearing and balance science through our Emerging Research Grants program. Please make a contribution today.