By Yehoash Raphael, Ph.D.
Flat epithelium is a condition where sensory hair cells and supporting cells in the cochlea are lost and the organ of Corti turns into a simple flat layer of cells, which can occur after a severe inner ear insult (damage).
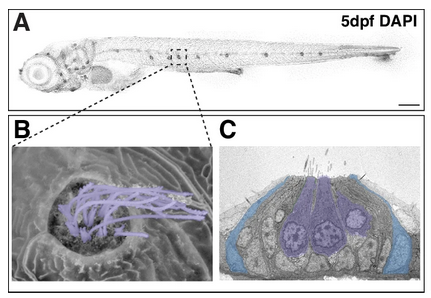
Whole mounts of the auditory epithelium stained with markers for actin (green) and Myosin VIIa (red) and photographed with epifluorescence. (a) In the normal auditory epithelium, one array of inner hair cells (I), 3 arrays of outer hair cells (1, 2, 3, indicating the 1st, 2nd, and 3rd rows), and pillar cells (P) are displayed. (b) Seven days after neomycin administration, the distribution of actin in adherens junctions between cells reveals a single layer flat epithelium of nonsensory cells with irregular apical outlines; whereas hair cells and differentiated supporting cells are absent. All images at the same magnification; scale bar = 50 μm. Credit: Liu et al./Hearing Research
The transcription factors (genes) Gfi1, Atoh1, Pou4f3, and Six1 (known collectively as GAPS) are important for the development and survival of hair cells. Previous research trying to regenerate hair cells in mature damaged ears by using a single transcription factor, Atoh1, produced very few cells. It also failed to produce new hair cells in severely injured organs of Corti, especially those with flat epithelium.
Studies in vitro suggested using combinations of transcription factors could be more effective than any single factor. We looked at the effects of overexpressing the GAPS genes in the ears of mature guinea pigs that were deafened and had flat epithelium. Our results were published in Hearing Research in November 2023.
The deafening was achieved by infusing the antibiotic neomycin into the inner ear fluid, causing flat epithelium and a substantial loss of nerve fibers. Seven days after deafening, adenovirus vectors carrying GAPS were injected into the inner ear scala media (cochlear duct) and successfully expressed in the flat epithelium.
One or two months later, we observed cells expressing the protein Myosin VIIa, which marks hair cells. Surprisingly, most of these cells were in regions under the flat epithelium, not within it. The number of cells, which we define as induced hair cells (hair cell-like cells), was not significantly different between one and two months.
Two months after treatment, we saw that some GAPS-treated guinea pigs had a statistically significant increase in new hair cell-like cells compared with controls. Additionally, qualitative observations indicated that ears with GAPS gene expression in the flat epithelium had more nerve fibers than untreated flat epithelium.
In summary, our results showed that overexpression of GAPS enhances the potential for generating new hair cell-like cells in a severe inner ear lesion model characterized by flat epithelium in the guinea pig, compared with using Atoh1 alone. But it remains uncertain whether these newly formed hair cells developed from the flat epithelium cells, as they appear to be situated in regions under flat epithelium (on the scala tympani side of the basilar membrane).
In addition, the new hair cells need to connect with nerve fibers to potentially restore hearing. We saw some promising signs of nerve regrowth, but more research is needed to determine if the new cells can signal to auditory nerves, even in their unusual location. Strategies to boost neuron survival alongside hair cell regeneration will also be important. Future steps will be to investigate the origin as well as the function of these hair cell-like cells.
Hearing Restoration Project members Yehoash Raphael, Ph.D. and Andy Groves, Ph.D., and their research teams are coauthors on the Hearing Research paper. Both Raphael and Groves are also former Emerging Research Grants scientists.






It’s ironic and puzzling that when going to hearing clinics, patients who need help with their hearing have to somehow hear and respond to staff.